Forewarning: This will be a lengthy post. I apologize in advance, but feel it is necessary to cover everything.
February 13, 2015. A day that will forever be engrained on my heart. I can’t believe it was already a year ago…
I was 19 weeks pregnant and on Thursday February 12, I had worked a very long 13 hour day…lots of meetings, clients, running around. I hadn’t drank a lot of water so I was dehydrated. I came home at 8pm with cramping and a backache. I had that tugging that I knew something was off. By 9pm I was having contractions that were measurable. I became terrified and called the doctor on call. She directed me to drink A TON of water and should be peeing every 30 minutes, to take a hot shower, and go to bed. She said if the contractions were still there in the morning, call back. I followed her directions and laid in bed praying that God would keep my baby girls safe through the night. I fell asleep and woke up the next morning, got dressed and drove into work.
On my way to work the contractions started back up and were just as strong. I called my boss, crying because I was so scared, and she sent me right home. I called the doctor back and they sent me right to the hospital to Labor and Delivery. I went to my mom’s house so I wouldn’t be alone and she drove me to the hospital. Zach was at work and wanted to come, but I assured him it was dehydration and they’d give me fluids and send me home.
My mom and I showed up to the hospital and they hooked me up to monitor my contractions. I was assigned the kindest and most amazing L&D nurse, Melissa. After an hour of monitoring and my contractions hanging around 7 minutes apart, they did a cervical check and I wasn’t dilated at all (thank God!). They did however want to do a thorough ultrasound with the Maternal Fetal Medicine Specialist to make sure the girls were okay, not in distress, and to see if there was an underlying reason I was having contractions at 19 weeks.
The ultrasound tech, Erin, was a Godsend. (God was allllll over this. From the contractions to every staff member… He had it down.) She was extremely thorough, assured me every step of the way and walked me through everything she looked at. She did tell me that there was something she wanted the Dr. to look at, however. So she called the doctor in, they read the reports and from there it was all a blur. I heard “A Vasa” “Baby A” “umbilical cord abnormality” “bed rest” “hospitalized” “c-section” “34 weeks” “hemorrhage” “I’m extremely concerned”…. I asked her to repeat this probably 10x. And then she left. I looked at my mom and said, “I just got bad news, didn’t I?” And she shook her head, yes. I was wheeled back upstairs to triage and Melissa came back and asked if I was okay. I told her I had no idea what was going on but I didn’t think I was okay. She called a doc from my practice to come and talk to me and there I learned the tip of the iceberg.
- The MFMS had pulled me from work for modified bed rest immediately.
- Nothing, and I mean ABSOLUTELY NOTHING was to enter my vagina…doctors, sex, foreplay, cervical checks…nothing.
- I would be hospitalized at 28 weeks for bedrest where I could be monitored frequently and close to an OR
- Steroid shots would be done to help prepare the girls’ lungs for an early arrival
- I would have a c-section scheduled for 34 weeks to ensure I wouldn’t go into labor
- Piper (Baby B) was safe
- Lila and my health were of the greatest concern
My mom took me back to her house and I started making the calls. I told my amazing boss that I had to be on maternity leave effective immediately… my doctors didn’t even want me working from home. They wanted nothing but cherries and rainbows..no stress, absolutely nothing that could possibly cause stress (ha, that had to be a joke right..I mean I was on bed rest for the safety of my girls!).
As I would later learn and through lots of research here is what I found:
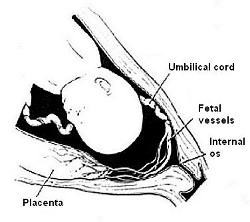
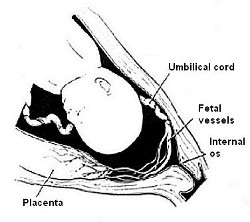
- Vasa Previa is a condition where exposed fetal vessels traverse the amniotic membranes between the baby’s presenting part and the internal cervical os, unprotected by placental tissue or umbilical cord. Basically, Lila’s umbilical cord at some point were exposed and those exposed vessels (2/3 for Lila) were laying across my cervix.
- It is rarely reported however has been estimated to occur in 1:2500 births.
- When undiagnosed, has up to a 95% mortality rate
- The biggest concern is the vessels tearing when the cervix dilates, rupturing if the vessels get pinched in the cervix, etc.
- Risk factors include: velamentous cord insertion, bilobed placenta, low lying placenta (check), pregnancies resulting in in-vitro fertilization (check with the meds), multiple pregnancies (check). I was at a higher risk.
- With diagnosis comes almost a 95% survival rate!!! PRAISE GOD!
- Diagnosis must happen with a transvaginal color doppler u/s
- Delivery must occur by cesarean section before labor begins
- Pelvic rest
- Hospitalization in the 3rd trimester (28 weeks with twins)
- Delivery by 35-36 weeks with singletons, 34 weeks with twins
- Immediate blood transfusion in the event of a rupture
- Steroid treatments at 28 weeks to accelerate maturation of baby’s lungs
The days and weeks that came following diagnosis were filled with so much anxiety and fear. I felt like I was entering into unknown territory, however, one thing remained constant. God was in control. There wasn’t a doubt in my mind that my contractions happened for a reason. I was sent to the hospital and was under amazing care from a group of extremely talented medical professionals. I was monitored frequently and had detailed ultrasounds at the MFMS… I can remember that whole time so vividly. In some ways it seems like it was last week. And other times it feels like it was years ago.
It was such a crazy journey…I’m so thankful for diagnosis and to have two beautiful, healthy, and happy 9mo. baby girls now. I thank God every single day for our safety and don’t take that for granted. I know our story isn’t the story of everyone who has the diagnosis of VP and I pray for these families daily. What is the most angering part of it all is that with diagnosis VP can be managed… it is a simple ultrasound that can be done.
If you are pregnant, ask your OB, ask your u/s tech… This simple check with the color doppler can save your baby’s life.
xoxo,
Lindsey
8 thoughts on “Vasa Previa: The Diagnosis”